In the fast-paced and intricate world of healthcare, clear and concise documentation is crucial for providing quality patient care. This is where SOAP notes come into play, offering a standardized and structured method for healthcare professionals to document patient encounters.
Table of Contents
What is a SOAP Note?
A SOAP note is a specific format used by healthcare professionals to document patient information in a standardized manner. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, which are the four components of a SOAP note.
Each section serves a distinct purpose in organizing and documenting patient encounters.
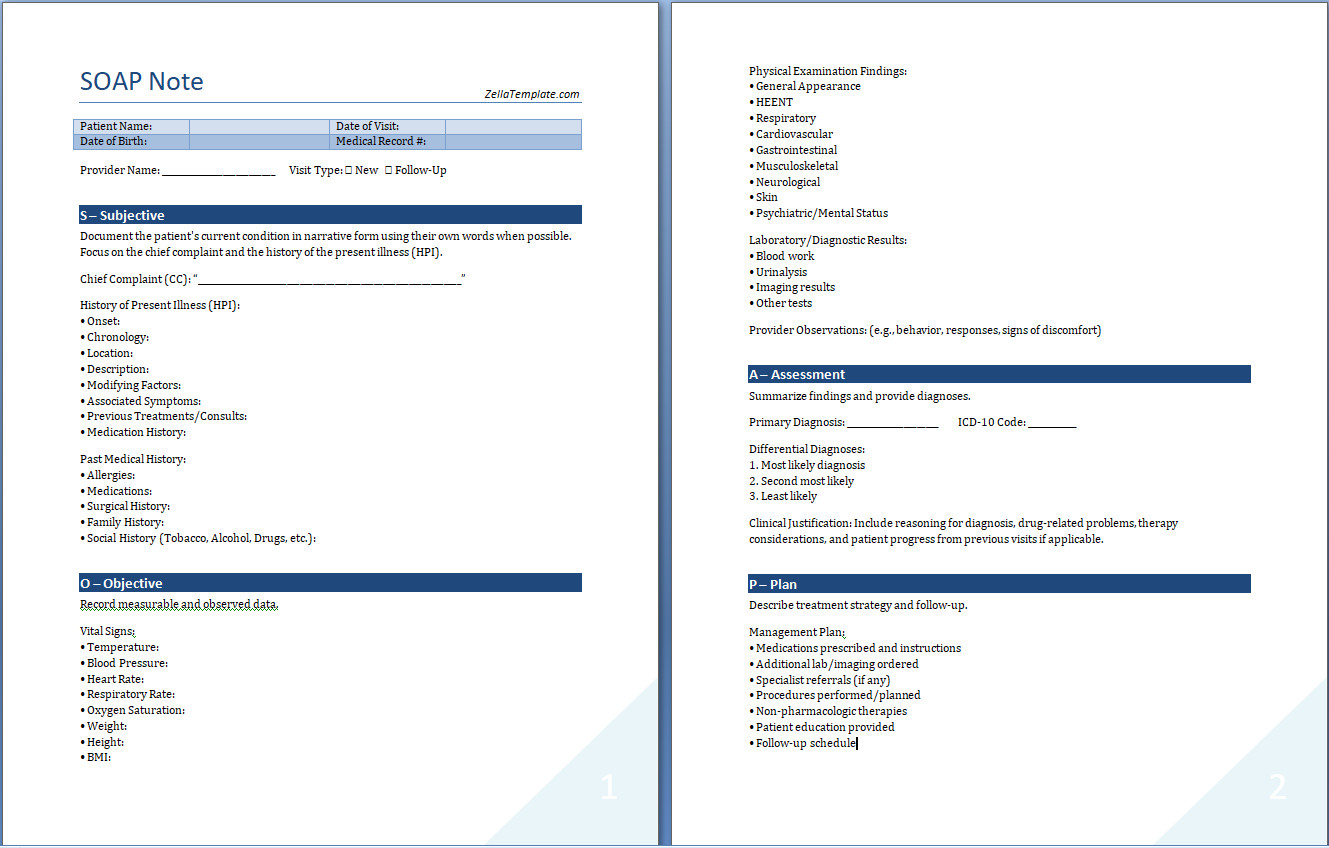
SOAP Note Example:
The Benefits of Writing SOAP Notes
Writing SOAP notes offers numerous benefits for healthcare professionals, patients, and healthcare organizations. Some of the key advantages include:
1. Clear Communication
SOAP notes provide a structured framework for documenting patient encounters, ensuring that essential information is communicated clearly and effectively among healthcare team members. Clear communication helps to prevent misunderstandings, improve coordination of care, and enhance patient safety.
2. Efficient Information Retrieval
By following a standardized format, healthcare providers can easily retrieve and review patient information when needed. This facilitates more efficient decision-making, continuity of care, and collaboration among interdisciplinary team members. Efficient information retrieval is essential for providing timely and effective patient care.
3. Informed Clinical Decision-Making
The systematic approach of SOAP notes allows healthcare providers to analyze patient data, make accurate assessments, and develop appropriate treatment plans. Informed clinical decision-making is crucial for delivering evidence-based care, monitoring patient progress, and adjusting interventions as needed to optimize health outcomes.
4. Legal Protection
Comprehensive SOAP notes can serve as legal documentation of the care provided to patients. In case of disputes, malpractice claims, or audits, well-documented SOAP notes can protect healthcare providers by demonstrating adherence to professional standards, guidelines, and best practices. Legal protection helps to safeguard healthcare professionals and mitigate potential risks.
5. Quality of Care
By documenting patient encounters in a structured and thorough manner, healthcare professionals can ensure that all aspects of the patient’s condition are addressed. This comprehensive approach leads to improved quality of care, patient satisfaction, and health outcomes. Quality care is essential for promoting wellness, preventing complications, and fostering patient-centered healthcare delivery.
Components of SOAP Notes
Each component of a SOAP note plays a crucial role in documenting patient encounters and guiding clinical decision-making. Here are some key considerations for each section:
1. The Subjective Section
The subjective section of a SOAP note should include a detailed account of the patient’s symptoms, concerns, and medical history as reported by the patient. Healthcare providers should document the patient’s chief complaint, present illness, past medical history, medications, allergies, and social history. It is important to establish rapport with the patient, build trust, and actively engage them in the care process to gather accurate subjective data.
2. The Objective Section
In the objective section, healthcare providers should document measurable and observable data gathered through physical examinations, diagnostic tests, and observations. This may include vital signs, physical exam findings, laboratory results, imaging studies, and other objective data relevant to the patient’s condition. Objective data should be recorded objectively, accurately, and comprehensively to provide a complete picture of the patient’s health status.
3. The Assessment Section
The assessment section involves the healthcare provider’s professional judgment and analysis of the patient’s condition based on the subjective and objective data. Healthcare providers should document their diagnoses, differential diagnoses, interpretations of test results, and ongoing assessments of the patient’s progress. The assessment should be logical, evidence-based, and reflective of the provider’s clinical reasoning and expertise.
4. The Plan Section
The plan section outlines the healthcare provider’s proposed course of action for the patient. It includes treatment plans, medications, referrals, follow-up appointments, and any additional tests or procedures needed. Healthcare providers should document their rationale for the plan and involve the patient in decision-making whenever possible. The plan should be individualized, evidence-based, and responsive to the patient’s needs and preferences.
How to Write SOAP Notes
To write effective SOAP notes, healthcare professionals should follow these best practices:
1. Be Clear and Concise
Use clear and concise language to document patient information in SOAP notes. Avoid using jargon, abbreviations, or vague terminology that may lead to misinterpretation. Clearly articulate the patient’s symptoms, physical findings, assessments, and plans straightforwardly and understandably to facilitate communication and promote shared understanding among healthcare team members.
2. Use Objective Language
Focus on objective data and observations in the SOAP note to support clinical decision-making and care planning. Use specific and measurable terms to describe the patient’s condition, physical exam findings, laboratory results, and other objective data. Objective language helps to ensure accuracy, transparency, and consistency in documentation, enhancing the quality and reliability of information recorded in SOAP notes.
3. Include Relevant Details
Document all relevant information in each section of the SOAP note to provide a comprehensive overview of the patient’s health status. Include pertinent details about the patient’s history, symptoms, assessments, treatments, and follow-up plans to ensure continuity of care and effective communication. By capturing essential information accurately and thoroughly, healthcare providers can make well-informed decisions, monitor patient progress, and deliver high-quality care.
4. Follow a Structured Format
Arrange the information in the SOAP note according to the standard Subjective, Objective, Assessment, and Plan format. Follow a structured framework to ensure consistency, organization, and completeness in documentation. By adhering to a standardized format, healthcare providers can streamline the documentation process, improve information retrieval, and enhance communication within healthcare teams, promoting effective collaboration and continuity of care.
5. Update and Review Regularly
Regularly update and review SOAP notes to reflect changes in the patient’s condition, treatment plans, or assessments. Ensure that the information documented is accurate, up-to-date, and reflective of the patient’s evolving health status. By reviewing and revising SOAP notes regularly, healthcare providers can track progress, adjust interventions as needed, and ensure that the patient’s care plan aligns with their current health needs and goals.
SOAP Note Template
Many healthcare organizations provide standardized SOAP note templates to guide healthcare providers in documenting patient encounters. These templates typically include prompts and sections for each component of the SOAP note, ensuring consistency and completeness in documentation.
Using SOAP note templates can streamline documentation, improve efficiency, and enhance the quality of patient care by standardizing documentation practices across healthcare settings.
SOAP Note Template – Word